Evaluating the Impact of the GCQ on the COVID-19 Pandemic in Metro Manila
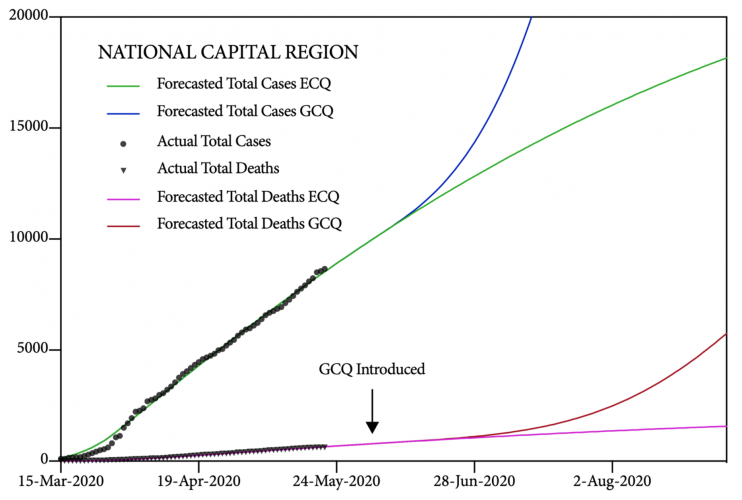
On June 1, 2020, the National Capital Region was moved from a MECQ to a GCQ. Since it has been two weeks since the NCR moved to this new level of quarantine – which is equivalent to a single incubation period for COVID-19 – we believe that this is an appropriate time to evaluate its impact on the dynamics of the local pandemic in Metro Manila.
Key Finding #1
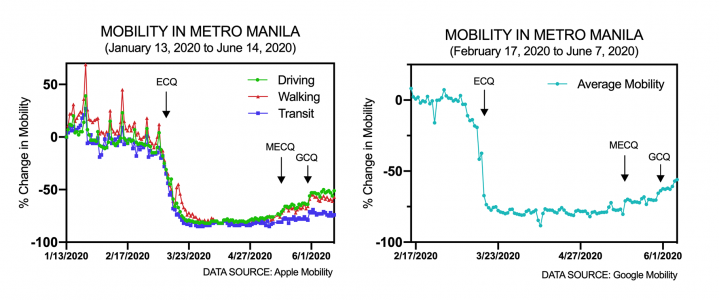
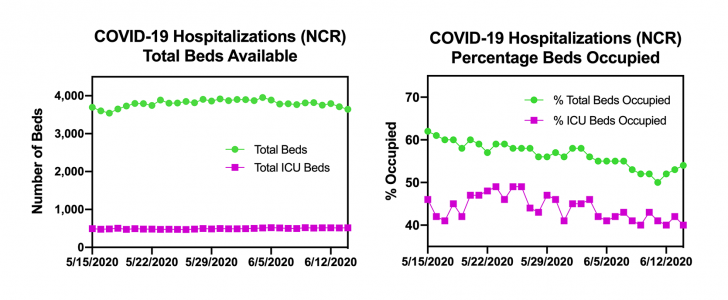
• The GCQ increased mobility in the NCR by about 10-15% from levels observed during the MECQ. Overall mobility in Metro Manila remains below 50% of levels recorded before the COVID-19 pandemic, as measured by Apple and Google.
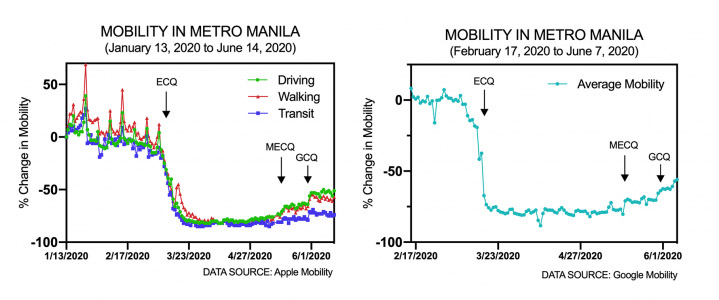
As shown in the left panel of Figure 1, the shift from the MECQ to the GCQ increased mobility in Metro Manila by about 10-15% from levels observed during the MECQ. Nonetheless, mobility levels, especially mobility on public transit, remain relatively low. They are more than 50% below baseline as measured by Apple during the first two months of the year. It also appears that the mobility levels of the GCQ have stabilized at driving (-53%), walking (-58%), and transit (-73%).
These low mobility levels at more than 50% below baseline are expected since the GCQ prohibits movement of those who are younger than 21 and those who are older than 60 years of age. Together, these two groups of persons constitute about 50% of the population of the Philippines.
To avoid selection bias, since it is not clear if Apple users are representative of the population in Metro Manila, we confirmed the Apple mobility trends using mobility data provided by Google. As shown in the right panel of Figure 1, the trends appear to be comparable. The average mobility as determined by Google for the five categories of locations it tracks in Metro Manila was -56% on June 7, 2020. Once again, the baseline is population mobility in the NCR prior to the pandemic.
Key Finding #2
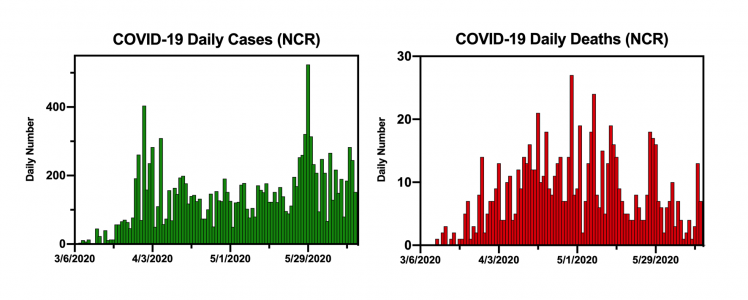
• Though there was an apparent spike in reported cases of COVID-19 earlier in June, we do not believe that this represents a surge in community transmission of the disease. The positivity rate in the NCR remains low and COVID-19 hospitalizations in Metro Manila are decreasing.
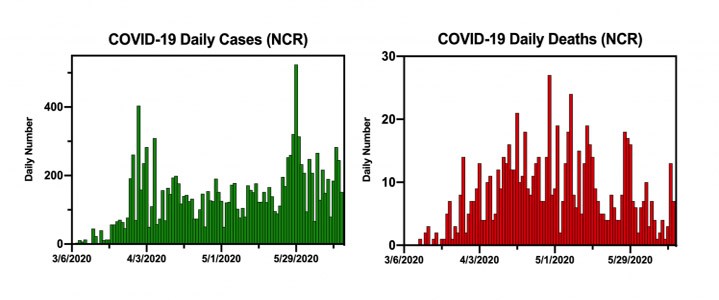
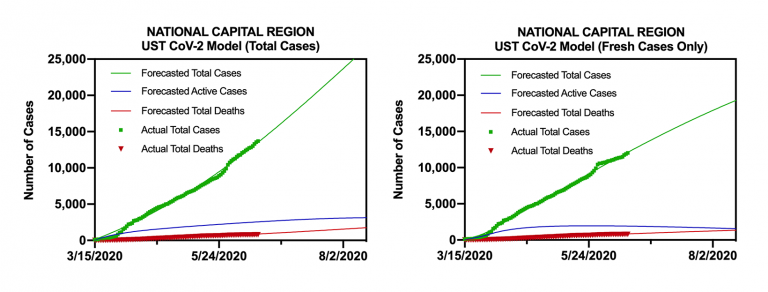
As shown in Figure 2, on the left panel, it appears that the number of daily cases of COVID-19 reported by the Department of Health for the NCR spiked earlier in June. However, it is not easy to interpret this spike because the DOH explained that their reported positive cases at the end of May and at the beginning of June included both “fresh” and “late” cases. Fresh cases were patients who received their positive test results three or less days prior to the reporting date and who were only recently validated. Late cases were validated tests for tests administered more than four days prior to the reporting date.
Furthermore, as shown in the right panel of Figure 2, we do not see a spike in the number of daily deaths in the NCR, even two weeks after the spike in daily cases. Deaths from COVID-19 lag behind reported new cases by about 10-14 days because of the incubation period of the disease. Indeed, it is hopeful that the number of daily deaths in Metro Manila continues to decrease from a peak in early May. The numbers of daily cases and daily deaths used for these graphs were those provided by the DOH on its COVID-19 tracker on June 15, 2020.
Therefore, to see if the spike in reported cases reflected a true surge of COVID-19 infections in the community, we calculated the positivity rate for Metro Manila for the past two months. The positivity rate is the percentage of total COVID-19 tests that are positive. If the pandemic is spreading silently within the population, we would expect the positivity rate to increase as more and more people become infected and some are then tested positive.
To calculate the positivity rate, we counted the total number of tests, positive tests, and negative tests reported by the DOH-licensed RT-PCR laboratories in the NCR as listed in the COVID-19 Philippine Situationer #044 published by the DOH. The numbers of tests were those provided by the DOH in its Data Drop for June 15, 2020. Tests with no clear result were ignored.
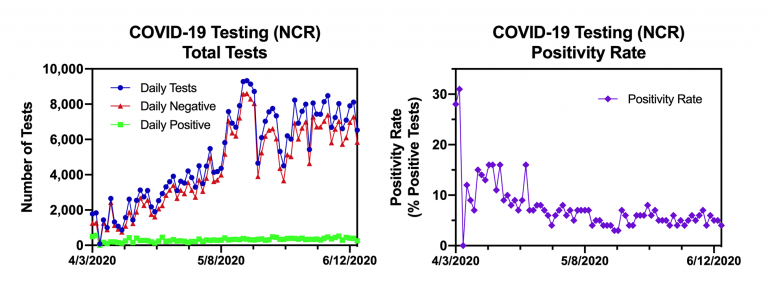
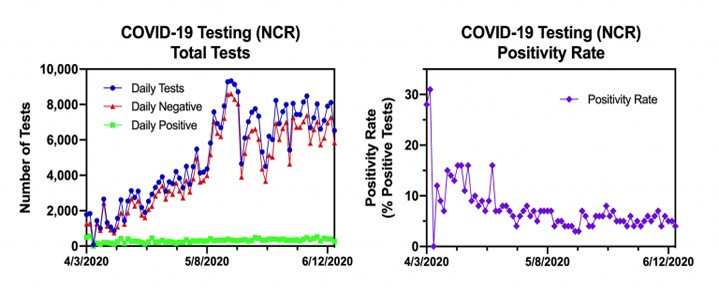
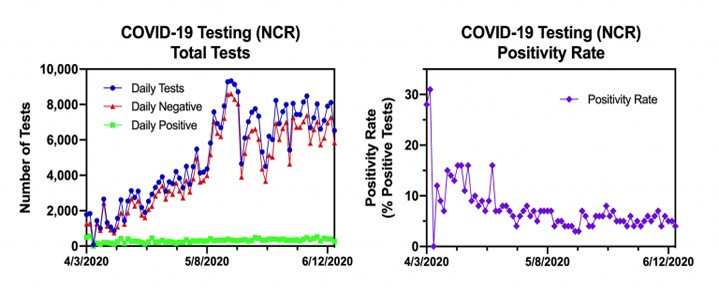
First, as shown in the left panel of Figure 3, it is clear that the testing capacity for the NCR has increased eight-fold during the past two months in Metro Manila. For the past two weeks, there have been around 8,000 tests performed daily at DOH approved laboratories.
Guidelines from the WHO published on May 12, 2020, indicate that countries should aim to test one out of every 1,000 residents every week and should see less than 5% of those tests come back positive for at least two consecutive weeks before they begin to relax social distancing and other public health measures. A low positivity rate indicates low community transmission.
As shown in the right panel of Figure 3, the positivity rate for Metro Manila has fallen from a high of around 30% at the beginning of April to just around 5% in early June. We believe that this indicates that community spread remains low despite the apparent spike in cases reported at the beginning of June.
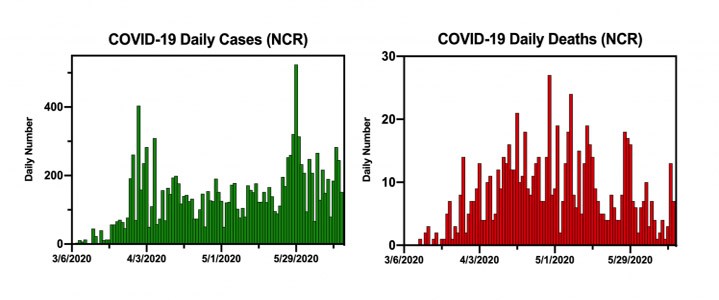
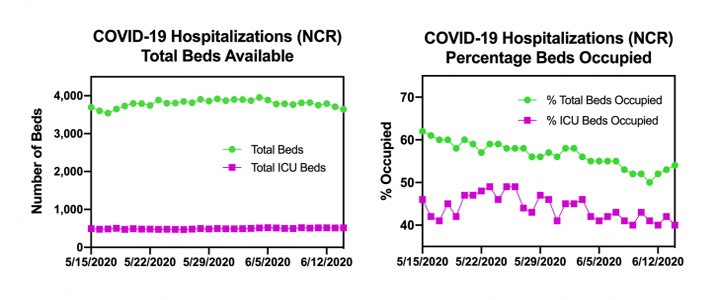
To see if the spike in reported cases reflected a true surge of COVID-19 infections in the community, we also determined the COVID-19 hospitalization rate for Metro Manila for the past month. If the pandemic is spreading silently within the population, then we would expect the hospitalization rate to increase as more and more people become infected and some are then hospitalized.
To determine the hospitalization rate, we counted the number of occupied and vacant COVID-19 beds and occupied and vacant COVID-19 ICU beds as reported by the hospitals in the NCR to the DOH, as these numbers were recorded in the DOH Data Drop for June 15, 2020.
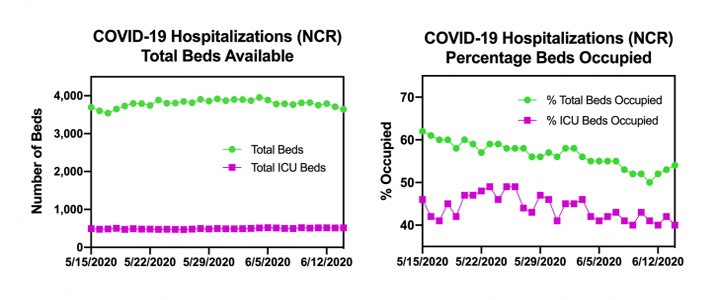
As shown in the left panel of Figure 4, the numbers of total beds and ICU beds available for COVID-19 patients have remained steady in the NCR. However, the percentage of both occupied total beds and occupied ICU beds for COVID-19 patients has gradually decreased over the past month. Once again, we believe that this indicates that community spread remains low in Metro Manila despite the apparent spike in cases reported at the beginning of June.
In sum, we conclude that the local pandemic in the NCR remains relatively subdued and controlled despite the move from the MECQ to the GCQ on June 1, 2020. The apparent spike in cases reported at the beginning of June appears to be explained best by changes in the DOH validation process of past cases, rather than by a surge in the number of infected patients.
Key Finding #3
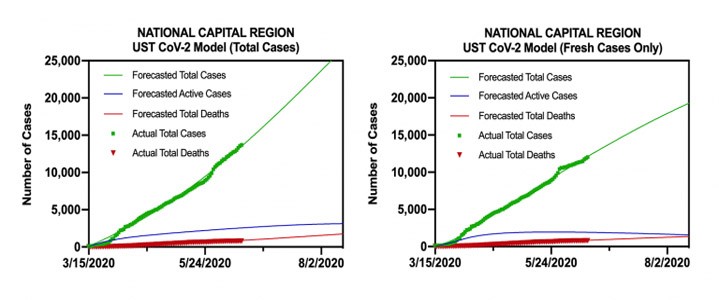
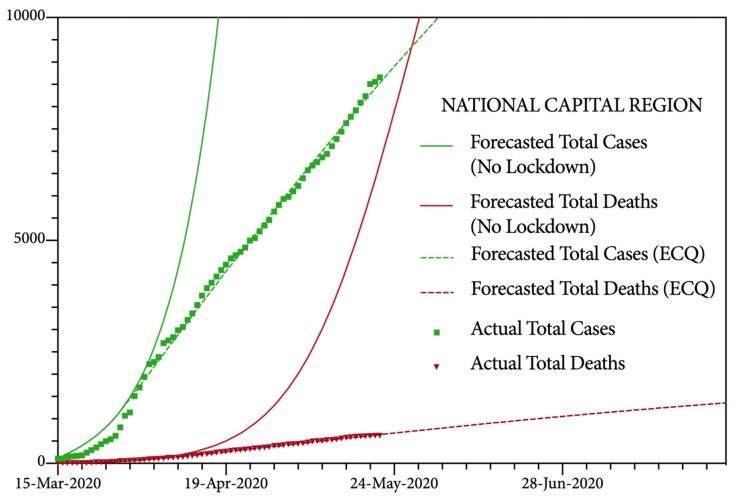
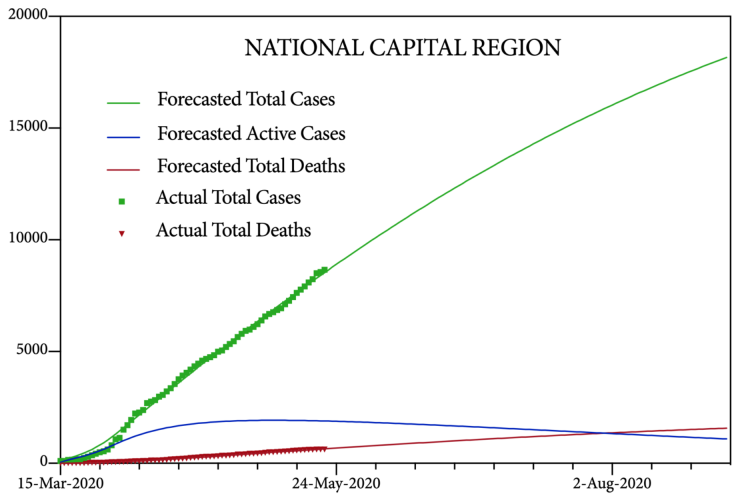
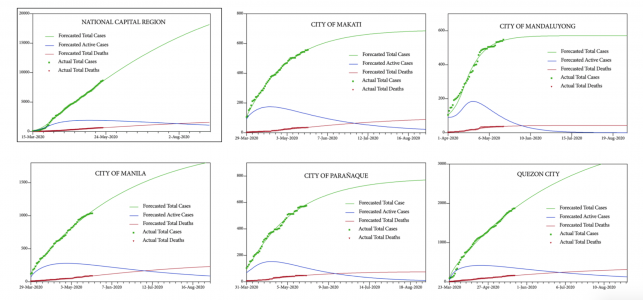
• Though it is difficult to properly forecast the progression of the local pandemic because of the uncertainty in the dating of the DOH data after June 1, 2020, we used our machine-learning UST CoV-2 model to determine future trends of the disease in the NCR.
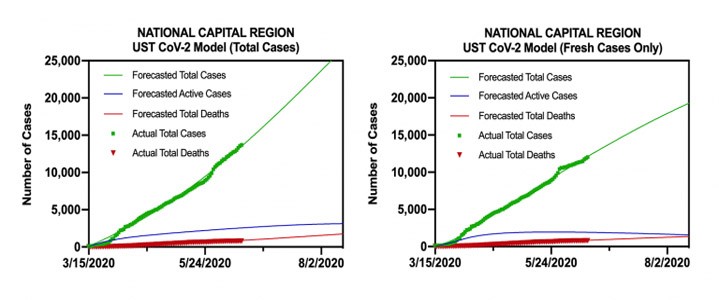
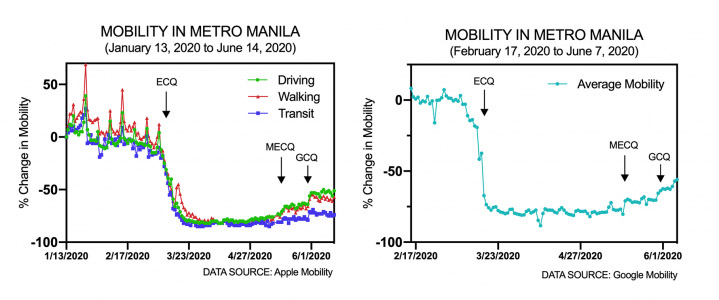
As shown in Figure 5, on the left panel, with the total daily case numbers provided by the DOH, we forecast that there will be 16,547 cases in the NCR by June 30, 2020, with 2,756 deaths. With total cases included, the modeled Reff = 1.1. However, as shown in Figure 5 on the right panel, when we repeated the modeling using only the “fresh” cases reported by the DOH, these estimates dropped to 14,032 total cases and 1,853 deaths. With only fresh cases included, the modeled Reff = 1.0.
Once again, because of the uncertainty of the DOH data, these numbers remain estimates that can give us a sense of the possible progression of the pandemic. Given our earlier analysis, we favor the second model that only includes the fresh cases since this forecast would follow from a controlled local pandemic.
Furthermore, we want to stress that these numbers are not inevitable. They can be reduced with robust testing and contact tracing programs. Consequently, we urge public health authorities to continue to increase and to strengthen both of these capacities in the National Capital Region.
Policy Recommendations
• Before Metro Manila is moved from a GCQ to an MGCQ, we recommend that the positivity rate should remain below 5% for at least another two weeks, and that levels of hospitalization in the NCR should continue to decrease, again for another two weeks, to indicate that the pandemic is not surging. This will also give local authorities additional time to increase both testing capacity and contact tracing ability to counter future outbreaks of this viral disease.
As we explained in our earlier report published online on this website on May 24, 2020, at this stage of the pandemic, according to the recommendations of a team from Harvard University, the NCR should have a testing capacity of 15,000 tests per day and 1,800 contact tracers working in call centers scattered throughout the region, to control its local pandemic. We do not believe that these recommended numbers need to be revised since they are based on deaths per day, and the number of COVID-19 deaths per day have been gradually decreasing for the past several weeks in Metro Manila. Deo gratias.
Finally, we encourage local authorities to continue to impose targeted lockdowns by zones to quarantine affected buildings, streets, and/or barangays that have elevated numbers of COVID-19 positive patients. This strategy of focused lockdowns should be coupled with extensive testing and tracking of contacts within these “high-risk” red zones to break chains of viral transmission. Recent studies have suggested that young persons who have COVID-19 – the population of the Philippines is young with a median age of 24 years of age – are often asymptomatic. Only testing for the virus using the RT-PCR approach will be able to identify these silent spreaders within the cities of Metro Manila.